It’s a search for a connection between asthma and respiratory syncytialvity
Clesrovimab: a Novel Antiviral Vaccine for the Treatment of Rare-Stage-Violet Influence in Children with RSV
“RSV has been a major cause of morbidity and mortality around the world, and I think this is going to change dramatically,” says Louis Bont, an infectious-disease paediatrician at the University Medical Center Utrecht in the Netherlands. Cost and infrastructure issues are likely to delay access to LMICs and he cautions that the benefits are unlikely to be evenly distributed. And even in wealthier parts of the world, broader questions have arisen about how to deploy these various preventive strategies in the safest and most effective way.
Providing a broad range of drugs for prevention could help health-care providers stay one step ahead of the evolution of the virus, because new versions might render some existing drugs obsolete.
One problem was that this vaccine preparation procedure seemed to lock the viral particles into a structural state that can elicit antibodies that bind to the viral proteins reasonably well, but that were not up to the task of neutralizing infection. In fact, some studies have indicated that the antibodies elicited by RSV infection following immunization with the formalin-inactivated vaccine could accumulate as immune complexes in the lungs, where they could subsequently promote a damaging inflammatory response.
It took decades of investigation and debate before researchers clarified the various factors that coalesced to inflict such damage. The vaccine-enhanced disease that the children experienced was created by a perfect storm, according to Varga.
In parallel, the inactivated virus seemed to do a poor job of training killer T cells, which would normally go on to eradicate virus-infected cells in future encounters. There was a crucial gap in the antiviral defences due to the immunological lapse. However, the vaccine did elicit a potent reaction from a subset of helper T cells that subsequently recruited a drove of other immune cells during infection, which could elicit a potent — and damaging — inflammatory response in the lungs.
clesrovimab has several design features that make it different from irsevimab. One important distinction is it’s target location. It takes a structural change in theprotein to access it, so irrimimab is only present in the spot on the apex. But, clesrovimab latches on to the protein’s flank, on an area that remains consistent across different conformations of the protein.
When we started the clinical programme with Suptavumab, we thought it was a really potent antibody and that it could bind to an extremely conserved site. But over the course of two years, just as Regeneron was running a clinical study across 18 countries and involving more than 1,150 preterm babies8, a new strain of RSV popped up that compromised the ability of suptavumab to neutralize one subtype of the virus.
After decades of disappointment, the arrival of two effective preventive therapies is clearly a cause for celebration — but unanswered questions remain.
Unless you have had cancer or experienced an inflammatory disorder, chances are you have never taken an antibody drug. But Oliver DeLong, a healthy baby from Chicago, Illinois, probably received his first antibody therapy before he was even four months old.
“What we have now is a situation where you can give a single shot of this highly potent antibody to an infant and protect them for an entire season,” says Tonya Villafana, head of nirsevimab’s clinical development at AstraZeneca, a drug firm based in Cambridge, UK. The company is now co-developing the drug with the pharmaceutical firm Sanofi, based in Paris.
The universal roll-out of antibody drugs by health-care systems is uncharted territory, unlike the commonplace practice of maternal vaccination against respiratory infections such as influenza and pertussis (whopping cough). The existing clinical infrastructure may be crucial in the successful adoption of either approach.
Steve Cunningham is a respiratory-disease specialist at the University of Edinburgh, UK. The debate is about the best coverage option over the next year or two.
It is not clear how much that price will be. But Michael Dunne, chief medical officer and head of development at the Bill & Melinda Gates Medical Research Institute in Cambridge, Massachusetts, expects it to be well below the $300 or more that drug companies will probably charge in Europe and North America for nirsevimab. “We’re going to get the price down as low as we can,” Dunne says.
Comparing the study of palivizumab and other vaccines to achieve universal coverage for low- and middle-income patients in the U.S.
Banerji has advocated for unrestricted access to palivizumab for Inuit babies born in remote northern communities. However, her appeals have gained limited traction.
Things should be different with nirsevimab. As a one-time, lower-cost option, nirsevimab should streamline the administration process, while also being “highly cost-effective or cost-saving as compared to the pilot strategy in Nunavik”, according to a 2021 modelling study led by researchers at York University in Toronto5.
The thing doesn’t have to be either. Catherine Weiss-Olivier said that each strategy has its own benefits, and that offering both could achieve maximal population coverage due to the variations in health-care systems and public acceptance of medical interventions.
As chair of the non-profit ReSViNET Foundation, an international RSV research consortium, Bont has worked with AstraZeneca and other pharmaceutical companies to evaluate most of the RSV vaccines and antibodies being considered for widespread roll-out. Although the two strategies have never been tested head-to-head, the antibody seems to be both more effective and potentially safer, he says.
On a molecular level, the Adimab agent — called RSM01 — and nirsevimab are fairly similar. Laura Walker, former head of science at Adimab, said that the antibodies bind to adjacent sites on the fusion protein and show comparable strength in laboratory experiments. The differences are not that big, she says. An important potential advantage can be found in RSM01. A non-profit biotechnology arm of the Bill & Melinda Gates Foundation plans to advance the drug and offer it in low- and middle-income countries for as little as manufacturing costs will allow.
As with most medical interventions, however, the first beneficiaries of nirsevimab will invariably be in wealthier parts of the world — that is, children such as Oliver.
The tragedy of 5 February 2010: a child died of respiratory syncytial virus in Kent, a possible link between asthma and RSV
Still, this doesn’t prove that RSV causes asthma in the long run, caution the authors. Doing so would require ‘probe studies’ — long-term randomized clinical trials involving interventions that can “take out the disease to see what happens”, says Anderson. This would mean having an RSV vaccine or treatment on hand — neither of which are currently available for infants or young children.
This article describes the death of a child. If you or someone you know needs support on this issue, please see
www.samaritans.org
for information.
It has been more than a decade, but Rachael Thomas still remembers the early hours of 5 February 2010 as if it was yesterday. She was standing against the wall in a hospital room in Kent, UK, watching a team of doctors fighting to save her 13-week-old child, Alexander. “They were putting tubes in him and silently crying,” she says. I remember thinking if the doctors were crying, it must be really bad.
At the hospital, doctors worked furiously to save Alexander, but stopped after 2.5 hours of trying to revive him. “I held him while they turned the machines off. I sang to him because I didn’t want him to be scared,” she recalls.
When the post-mortem results came through, it was found out that Alexander had died of the respiratory syncytial virus. The virus causes a highly contagious infection of the lungs and respiratory tract. It can strike at any age, but young children are most at risk. The virus can pass with little consequences after a week or two. If you’re born premature, or someone has an underlying illness, RSV can cause serious consequences, such as pneumonia and bronchitis.
The question when these symptoms persist for a long time is whether they are a disease or not. But for now, scientists are unsure how much credence they should give to the idea of ‘long RSV’.
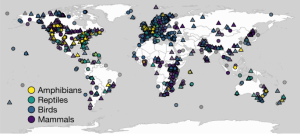
Source: The search for a connection between RSV and asthma
The Impact of Long-Term Follow-up on the Prevalence of Tramadoxetine Efficacy in Low-Income Countries
“That made us think that we should include long-term follow-up in our studies,” he says. The research started after palivizumab entered the market.
We would like to acknowledge the financial support of Moderna. As always, Nature retains sole responsibility for all editorial content.
Even as these developments result in optimism, substantial hurdles remain. People in low income countries are especially vulnerable due to the inequalities of access to existing interventions. Without policies to ensure equity, some communities could be left exposed.
Efforts to prevent infections and keep vulnerable people out of hospital are beginning to pay off, but deploying these strategies presents new challenges.