Many Americans may lose coverage in the future, but are not aware of it
When Medicaid Suspensions First Start to Move, People Will Not Get Their Renewal Notice – Samuel Camacho: What Did Ohio Do Before the Pandemic Drop?
GODOY: Ohio has already started sending out renewal packets. At least 200,000 people in the state are expected to lose coverage starting in April. But that’s just the people who will no longer be eligible. The state cannot reach many who are eligible for Medicaid, which will result in them being dropped.
MARIA GODOY, BYLINE: Before the pandemic, people often got dropped from Medicaid, not just when they were no longer eligible but because keeping your coverage involves a lot of red tape. It’s a lot of work. So when Congress passed a law prohibiting states from dropping Medicaid recipients, it was a relief for many low-income people.
“That’s been really important because you don’t want to find out that you don’t have Medicaid when you are in the emergency room,” says Bamberger, who heads a team of health insurance navigators.
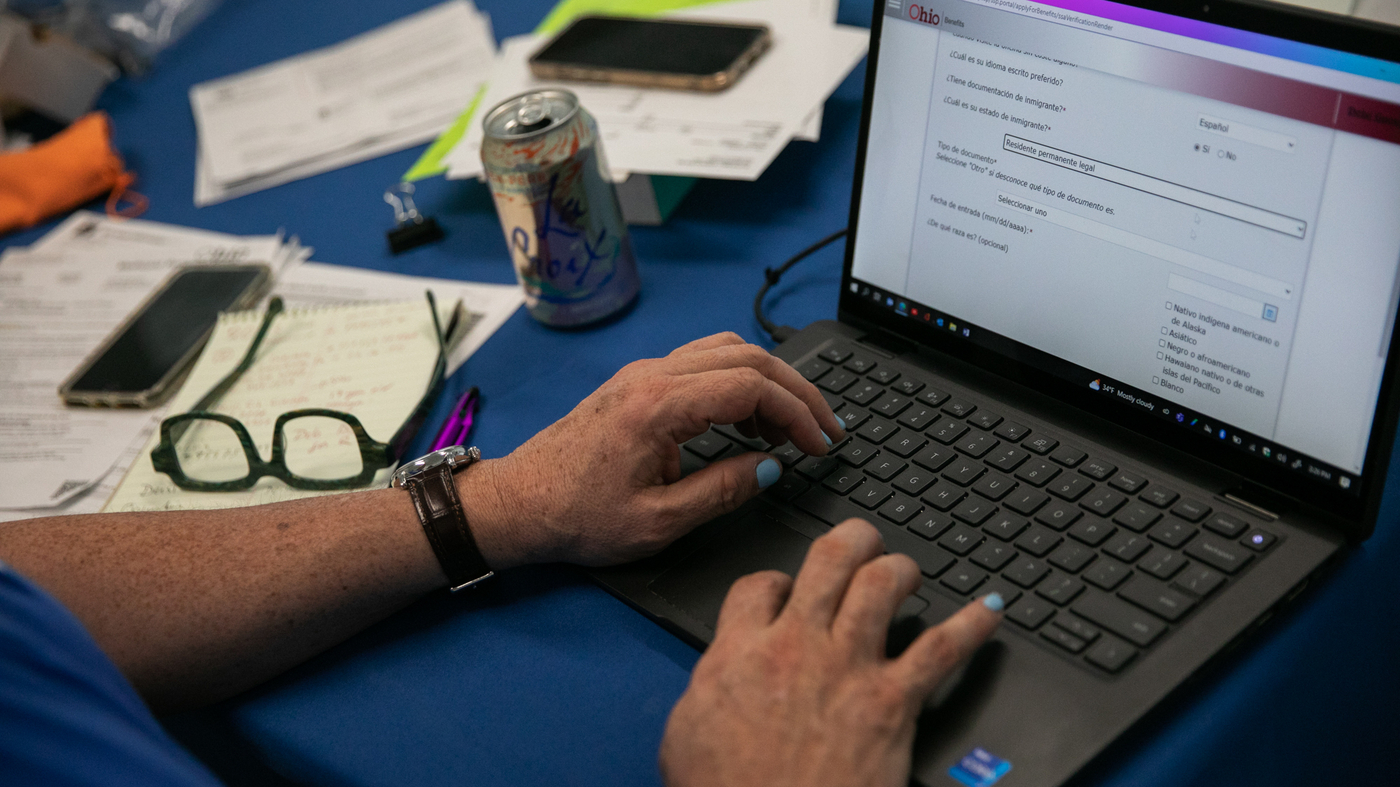
GODOY: Many people have moved since the last time they had to renew their Medicaid three years ago, so they may not get their renewal notice. Samuel Camacho is a health insurance navigator with the Universal Health Care Action Network of Ohio. He says language is another major barrier.
A Spanish Speaker During the Pandemic. She explains why she is worried about her job, but she realizes she doesn’t exist
Good morning, God. She has to provide documentation to show that she no longer works at the nonprofit job she left over a decade ago. That organization doesn’t exist anymore.
GODOY: Still, he’s relatively lucky. She knows that she needs to renew her Medicaid soon. According to a survey from the Urban Institute, most Americans don’t know they need to act to keep their Medicaid coverage. Some people don’t realize they have lost Medicaid coverage until they actually need it.
Camacho helps Spanish speakers in the Columbus, Ohio, region. He says that the process has become harder because the agency that handles Medicaid have closed their doors to the public.
CAMACHO: Before the pandemic, individuals were able to go to the offices with an interpreter and have conversations with their case managers, print documents, find documents in their language, have interactions with people, even other Medicaid recipients. We have lost that.
Re-enrollment of a U.S. Medicaid Patient: Dominique Jackson, a Columbus resident, discovered his Medicaid cards early in the morning
CAMACHO: You know, the bill that you send was under your husband’s name, but it needs to be under both of your names, little details. Those details are what get denied if they aren’t taken care of.
NPR transcripts are created on a rush deadline by an NPR contractor. The text may change or be revised in the future. The accuracy and availability of things may be different. The authoritative record of NPR’s programming is the audio record.
Dominique Jackson has been on Medicaid for seven years. But the Columbus, Ohio, resident didn’t realize he’d have to verify his eligibility every year to keep his coverage. He injured his ankle.
“I found that I had to re-enroll because I went to the emergency room and I still had my old Medicaid card. And when they scanned it, it came up that I was no longer under that provider,” Jackson recalls. He was able to file the paperwork and have his care covered.
This was one big reason behind historically high rates of Medicaid enrollment and an all-time low rate of people who were uninsured in the U.S. last year.
That includes nearly 7 million people who remain eligible for the program but face barriers to filling out their paperwork in a timely manner, according to projections from the Department of Health and Human Services.
But it will take some time and will not happen all at once. The states have the ability to restart the process differently. The majority of states plan to do it over the course of a year, according to a report.
It is bound to be a messy and difficult process. The process of re-enrolling is not easy, starting with the fact that they may not get the notification they need to do it, as well as difficulty in obtaining the necessary documentation.
What happens when you’re not able to get a check from your old girlfriend or boyfriend, or that’s the hardest part of it all: How difficult is it to get verification?
“You’ve got a disproportionate number of people here who are not computer literate and whose housing is unstable,” Bamberger says, adding, “Just because I listed my friend as a mailing address three years ago doesn’t mean that that person’s going to keep my mail so that I can get it now if I’m homeless. [Or] what if that address is for your old girlfriend or boyfriend, and you haven’t spoken in two years?”
She points out that it’s difficult to get verification if your job doesn’t have a pay stub or if you work in the gig economy. They receive payment information on their phone. It doesn’t look like a pay note for someone who works in an office.
This process has been encountered firsthand by Ms. Jorgensen. “Gathering all of the verifications is like the most stressful part. It’s a job,” she says.
Source: https://www.npr.org/sections/health-shots/2023/03/21/1164849111/medicaid-renewals-are-starting-those-who-dont-reenroll-could-get-kicked-off
Language barriers to health insurance: Do Medicaid renewals are starting those-who don’t enroll-could-get-kickked-off?
Jorgensen lives in Columbus, Ohio. She’s spent much of her career working in social services nonprofits. She’s also a single mother of two on Medicaid, and is currently unemployed while finishing a certification in graduate school. She says that despite her expertise, it takes a lot of work to navigate the system.
People are expected to call us from the pharmacy in April. “That’s where they learn that my Medicaid doesn’t work.”
Samuel Camacho, a health insurance navigator with the Universal Health care Action Network of Ohio, says language is one of the major barriers to health insurance. Individuals are going to be vulnerable because of their lack of English. So they may receive a letter, but they can’t read it,” he says. Navigators like Camacho guide people in signing up for Obamacare, but they can also assist them with Medicaid.
Source: https://www.npr.org/sections/health-shots/2023/03/21/1164849111/medicaid-renewals-are-starting-those-who-dont-reenroll-could-get-kicked-off
Los Dias de Desafios: El Mundo a la Comunicada de Los Latinos, Además de los Diagresos
He says that kind of word of mouth is really important for the Latino community he works with. “Latinos – we’re a group that thrives on communication. ‘Abuelita le dijo a Titi, Titi le dijo al primo y el primo me lo dijo a mi.’ [Grandma told auntie, auntie told the cousin, and the cousin told me.] We’re losing that.
In his experience those denials happen more often than not. Even though they’re usually reversed on appeal, it’s frustrating to be doing it over and over again. It doesn’t make sense.
He says he just went back to normal after his battle with cancer. “Without the Medicaid, I don’t know how I would’ve been able to pay – it would have to completely have come out of pocket for the price of the medicines and treatments.”

