The power of non-pharmaceutical interventions is known as pain
The gut microbiome and endometriosis: how many years do we need to go through? A gynaecologist’s perspective
There are black blisters, red nodules, and white-hot cysts. They grow throughout the body, from the urethra to the peritoneum.
If detected, the endometriosis can be taken care of. For up to half of those who choose this, the pain returns and they need another surgery within five years. “As surgeons and doctors, we want to remove lesions. Amiraquedo, a gynaecologist who runs clinical trials at the university says that people’s pain persists more often than we like to report.
The pain experienced by people with endometriosis is vastly different from the pain experienced by other people. For some, it gets worse during their period while for others, it doesn’t go away all month long. It can be anything from vaginal, bowel and bladder pain that spreads to the floor and beyond to scorching muscle spasms.
This persistence of pain after the original stimuli have subsided or been removed is a key feature of many kinds of chronic pain. In some whole-body pain conditions, such as fibromyalgia, there is no clear cause. The pain system has been overwhelmed by a problem, leading to a desperate search for relief.
Despite these challenges, researchers are keeping an open mind that the gut microbiome could help to ease chronic pain. So immense is the burden, Maddern says, that “everything is worth trying at this point”.
John Cryan, a stress biology researcher at University College Cork in Ireland, said that there has been a slow evolution to recognize the role of the gut microbiome in the treatment of IBS.
Most studies capture only a snapshot of the gut microbiome. Cryan says large, longitudinal studies are needed to track microbiome changes in response to symptoms and treatment. His research in animals shows that early life stress affects the gut microbiome in ways that lead to persistent visceral pain in adulthood, even though the microbiome itself recovers17. He talks about the possible reasons why the kefir is not a reflection of the pathology of pain.
Maddern studies nerve pathways in visceral pain. Coming to this research some 20 years after her own endometriosis diagnosis, she was shocked at how little was known about pain and how to treat it. Only in the past few years have researchers begun modelling visceral pain in animal models of endometriosis, as they do for IBS. That’s because most endometriosis research has so far focused on understanding what causes the disease and the growth of lesions, rather than its pain.
This makes sense: people with endometriosis have an abundance of anaerobic bacteria sensitive to metronidazole in their gut. However, neither study looked at pain. So Quevedo and her colleagues at the University of Louisville Hospital in Kentucky are investigating whether administering endometriosis after surgery could reduce pain.
In a 2023 study, the team found that people with fibromyalgia also had lower levels of specific bile acids in their blood compared with healthy controls15. These secondary bile acids are produced by gut bacteria that people with fibromyalgia tend to lack. They reported more intense pain when the bile acids were lower, probably because some of the acids bound to the spinal cord suppressed the pain. Pain could flare up without them. The study suggests that restoring the levels of these bile acids could help to reduce fibromyalgia pain.
Pain and opioids in the 21st Century: From Pacira to the Optical Device of Day, Beyond the NHS, to Brain and Blood Tests
People spend a lot of time trying to help their physical pain. The world’s over-the-counter painkillers market was valued at nearly US$28 billion in 2022, and is predicted to grow to almost $41 billion by 2032. At the same time, the massive overconsumption of pain-management opioid drugs, which can be addictive, continues to shatter lives.
The financial support from Pacira is something we are grateful for. As always, Nature retains sole responsibility for all editorial content.
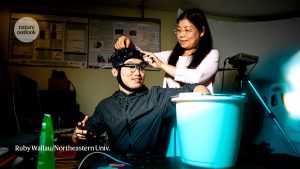
It needs a more nuanced understanding of what pain is to be able to improve it. Pain-o-meter devices are emerging that could finally bring precision and objectivity to every carer’s first question: “where and how much does it hurt?”. They’re looking into whether brain scans and blood tests are capable of predicting which treatments will work best in people with chronic pain.