biomarkers could mean a better pain treatment
A collaborative health outcomes information registry for chronic pain management in the United States, and a multi-dimensional perspective on the experiences of people with chronic pain
“You have to give each drug at least six weeks to see if it works, before trying the next one,” Russo says. Side effects can occur if the drug is used to relieve the pain. After cycling through each migraine drug individually, the team started testing drug combinations. She was able to control her migraines after the 24th medication trial.
The collaborative health outcomes information registry was developed in the United States. Since it launched in 2012, CHOIR has enabled pain clinicians to collect high-quality pain data in a standardized form from individuals. The platform, which tracks how people respond to each medication they try, has been adopted by clinics across the United States and beyond. Later this year, it will relaunch with the capability to include biomarker data in addition to its current offerings of demographics and symptom patterns. To capture a person’s experience of pain, it is important that we look at a person as a multi-dimensional being and build models that can predict treatment response.
Many researchers now hope to bring a level of objectivity to the diagnosis of pain by using devices that eliminate the social and individual variables that contribute to the current inaccuracies. According to Jeffrey Mogil, a pain researcher, people have been interested in pain for a long time. “It’s a huge priority.”
An optimistic person who breaks their arm mountain biking on a weekend away with friends to celebrate a promotion could experience pain differently to a pessimistic person who breaks an arm cycling from their monotonous job to their home, on which they are behind on the mortgage repayments. There is risk for the start of chronic pain from anxiety and depression. “Nobody experiencing chronic pain is in the same place at the same time,” she says. “That pain is situated in a milieu of everything else going around them, everything they’ve previously experienced, everything they’re anticipating, and all the emotions involved in that experience.”
Pain Detection using Deep Learning and Multimodal Data: A Case Study of the IMI-PainCare Biopain Consortium
Washed out to the human eye, at least. “When we compared the EEGs of people with pain versus those with no pain, standard statistical analysis showed no difference,” Saab says. When the machine learning process was trialed, the artificial intelligence of the engine used to process the data would detect something. The system could tell between people with chronic lower back pain who would benefit from a spinal- cord stimulator and people who wouldn’t, even if they hadn’t used a stimulator. The algorithm had an of accuracy almost 80%, Saab says, showing that even a simple AI can outperform conventional statistics for the task. “Basic machine learning is picking up signals that classic methods and the human eye are not capable of detecting.”
Vollert and his team have been able to identify three different groups of people by using machine learning to get a picture of their pain sensitivity.
The early results were promising. “In 2012, when I first published work using structural brain imaging to classify the presence or absence of lower back pain, we got 76% accuracy,” says Mackey5. Progress then stalled. The accuracy hasn’t improved since that time.
A stronger signal should emerge when the data from multiple techniques is pooled. The IMI-PainCare Biopain consortium led by Rolf- Detlef Treede, a neuroscientist at the University of Mannheim is one of two such efforts in Europe that Vollert is currently participating in. Prospective data sets that collect all of the same marker information in parallel from the same patients are needed to build good models. “That’s the kind of data set that we’re generating at the moment.”
With multimodal data in hand, advanced AI tools that are more powerful than the simple machine-learning models previously deployed will be crucial to categorizing people into subgroups and treatment selection, says Vollert. “We are working with machine-learning specialists to find models that go much deeper into these huge, rich data sets,” he says.
The latest advanced AI models — including ChatGPT and the AlphaFold protein folding prediction tool — use a machine-learning approach called deep learning neural networks. The models take an input data set and connect it to other data points to generate their output. Combining deep learning neural networks with big data sets will allow more fine-grained patient stratification and will result in accuracies significantly higher than 80%.
One caveat is that these advanced AI techniques apply non-interpretable models to biomarker data analysis. “In my early work with machine learning, I could tell you exactly what brain regions were contributing to the model,” says Mackey. I can’t tell you what’s driving it, we can get incredible accuracy with the new and improved versions.
Non-interpretable modelling presents a problem for pain-medicine practitioners, Mackey says. “As clinicians, we want to understand the basis of a medical recommendation and not just blindly take the word of a machine — because what if the machine is wrong?”
It took three long years for her to find a way to control her migraines. The problem was not a shortage of options — there are plenty of treatments for people with chronic migraines, Russo says. Even though it’s not easy to find the right treatment for every person with chronic pain, there are still many different options to choose from.
Her ferocious migraines would strike with daily frequency. “She would vomit and have to lie down between patient consults,” says Marc Russo, a pain-medicine physician at Hunter Pain Specialists in Broadmeadow, Australia, who treated her in consultation with a neurologist. “Then she’d have to get up, rinse her mouth and see the next patient.”
Continuous Objective Multimodal Pain Assessment Sensing System (COMPASS): An algorithmic approach for fine-tuning and management of chronic pain in people with chronic back pain
Lin acknowledges that the work is still not really working. Maybe we should stop. I don’t need an objective measure to tell me that the pain has stopped as I withdraw my hand from the cold.
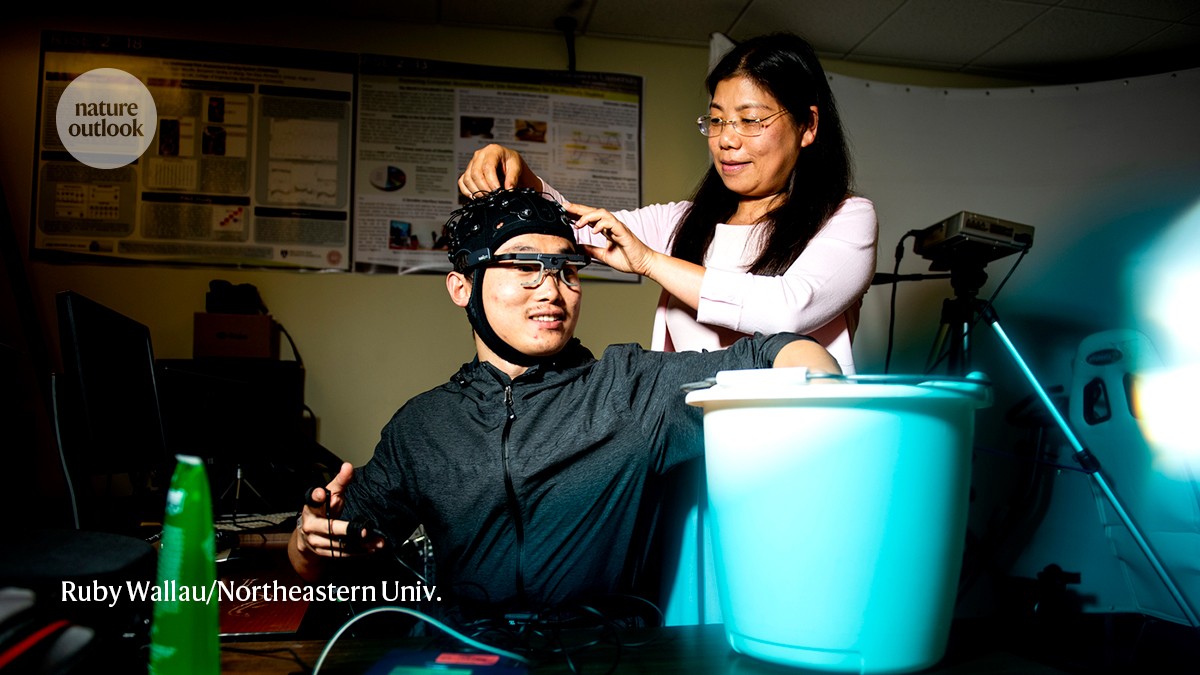
There was a glitchy platform. With my hand submerged in a bucket of ice water, the objective pain scores displayed on the app generally trended upwards. The readings were inconsistent, however, fluctuating as I experienced a steadily increasing sensation of pain.
When I was trying the cold exposure task in the lab, I had only one sensor on my body. Recording facial tracking, pupil diameter and brain activity wasn’t done.
The researchers found that an inference from nine measures, which included facial expressions and brain activity signals, was better than other approaches, when evaluated against self-reported pain scores. Front. Neurosci. 16, 831627; 2022).
Lin has been fine-tuning her platform called Continuous Objective Multimodal Pain Assessment Sensing System (COMPASS) using data from people with chronic low back pain to validate her group’s machine-learning algorithms. Artificial-intelligence tools are more efficient at gathering data than any single mode, as they are able to provide insights that align with people’s own pain assessments.
A snapshot of a person’s pain can be provided by the technology offered by AlgometRx. For an assessment by a physician it can be fine, but it’s not possible to track the change in pain levels over time.
Costs and complexity make these methods unsuitable for clinical use. It has to be portable and simple to use.
The platform is authorized in the United States only for use during surgery with people who are under anaesthesia and unable to communicate their pain levels. The goal of this is to allow clinicians to adjust the dosages of the painkillers in line with the individual’s pain.
Moreover, many individuals — including babies, people who are non-verbal, people who are critically injured and those under sedation — cannot communicate their symptoms effectively. This further complicates the management and treatment of pain, and hinders the delivery of appropriate analgesia.
As discomfort escalates to pain, a sensor strapped to my chest detects changes in my heart rate, breathing pattern, skin conductance and other bodily responses. These physiological signals are processed through advanced algorithms to generate a pain score. My pain level is 4 and displayed on the app.
The graduate student bears down on my arm with a force akin to a firm handshake. The sensation gradually starts to hurt when concentrated on a small patch of skin, but this pressure might not seem like much.