A guide to acute Kidney Injury
Early Detection of Kidney Illness and Gravestitis Violation can Reduce the Risk of Death for Patients with AKI
People who spend time in hospital hope to leave healthier than when they arrived. But people undergoing surgery or treatment for severe injury or illness face the risk of acquiring covert damage to their kidneys that could have lifelong consequences, or even result in premature death.
Even mild AKI might increase the risk of death for people in hospital. The odds of death are six-fold higher in the most severe cases. AKI also increases the chance of stroke and heart attack.
It’s very important that we develop better diagnostic tools and risk-assessment tools to detect AKI early and give clinicians the chance to step in earlier. Researchers have identified biomarkers that can be spotted sooner than the physiological indicators currently relied on to diagnose AKI. Existing markers should be left clear for a short time so that damage can be repaired before it gets worse.
Predicting Acute Renal Injuries in Women with a New Nephron Transplant Algorithm: An Empirical Study
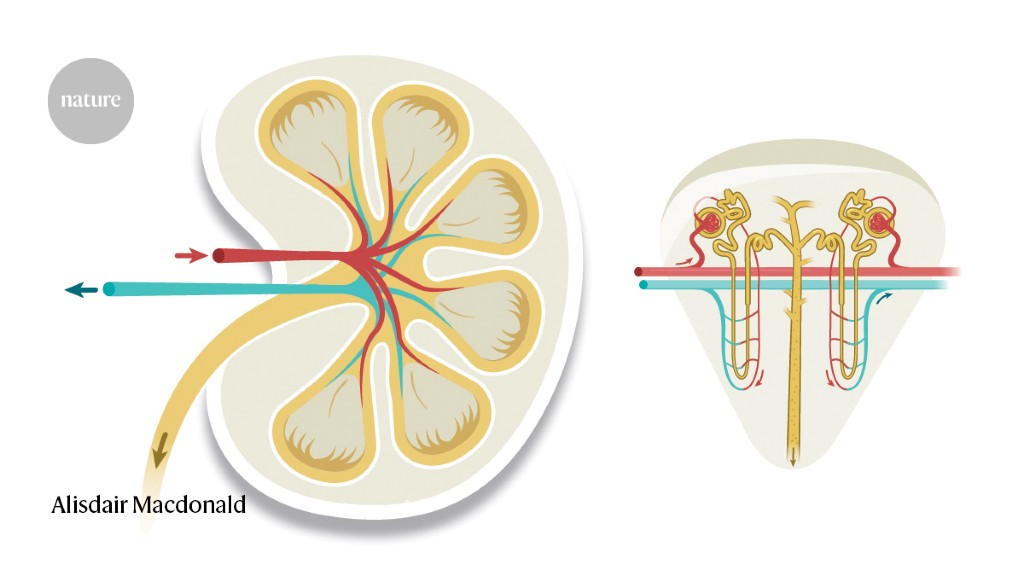
The kidneys help purify the blood and excrete metabolism out of it. At the heart of this purification system are hundreds of thousands of tubular structures known as nephrons.
Everybody is born with a finite number of nephrons, which then declines as we age. This means that older people are more vulnerable to the effects of nephron damage, because they typically have fewer healthy nephrons at the onset of injury.
Acute kidney injury (AKI) describes a range of conditions in which nephrons are damaged, impairing their function and reducing the efficiency of filtration through the glomerulus.
Up to 48 hours in advance, a algorithm was able to predict 90 percent of AKI cases that would require a transplant. Predicting in women is worse than in men, probably because of a lack of representation in the training data.